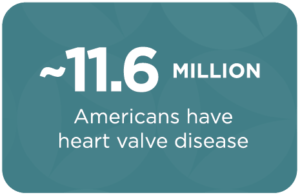
As many as 11.6 million Americans are estimated to have heart valve disease, and each year around 25,000 people die from the disease. Fortunately, valve disease can usually be successfully treated in patients of all ages.
But successful treatment depends on understanding risk factors, recognizing symptoms, and getting timely treatment. Unfortunately, three out of four Americans report knowing little to nothing about the disease.


How Does the Heart Work?
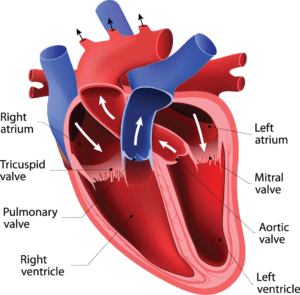
The heart is a powerful organ that is responsible for continuously circulating blood throughout the body. The heart’s four chambers squeeze and relax in a coordinated manner to pump blood to the lungs, and through the circulatory system to deliver oxygen and nutrients.
Between each of the heart’s chambers is a valve—a thin leaflet of tissue that keeps blood moving in only one direction and with the right amount of force. The valves keep blood from leaking backwards by only opening one way and sealing tightly as soon as blood passes through.
What is Heart Valve Disease?
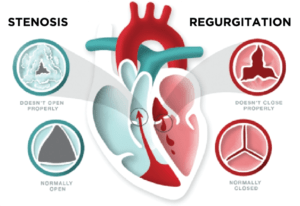 Heart valve disease (valve disease) is a type of heart disease that involves damage to one or more of the heart’s four valves that causes them to not open or close properly and disrupts blood flow. While some types of valve disease are not serious, others can lead to major complications including death.
Heart valve disease (valve disease) is a type of heart disease that involves damage to one or more of the heart’s four valves that causes them to not open or close properly and disrupts blood flow. While some types of valve disease are not serious, others can lead to major complications including death.
If a valve doesn’t close completely and allows blood to leak backwards, it’s called regurgitation or insufficiency, and may be referred to as a leaky valve. If a valve doesn’t open fully to allow enough blood to flow through, it’s called stenosis and may also be referred to as a sticky, narrowed, or stiff valve. A valve may also fail to open fully due to an obstruction.
Each of the heart’s four valves can have regurgitation or stenosis, or both—although the aortic and mitral valves are the most likely to be damaged. The most common types of valve disease are mitral regurgitation, mitral stenosis, aortic regurgitation, and aortic stenosis.
Depending on the type of valve disease, the damage can cause the heart to work harder than it should and can restrict blood flow to the rest of the body. Without treatment, this can lead to serious complications including arrhythmias, congestive heart failure, stroke, other heart disease, and even death. These complications can significantly impact quality of life, make everyday activities difficult, and lead to disability and loss of independence.
Who Is at Risk?
Valve disease is usually caused by wear and tear, disease, or damage. The most common risk factors for valve disease are:

Older Age
Wear and tear to the valves is the most common cause of valve disease. It can be caused by calcification—the gradual build-up of calcium that hardens and thickens on the valve and most commonly affects the aortic valve (aortic stenosis). It can also be caused by degeneration—the slow breakdown of the leaflets and attachments and that most commonly affects the mitral valve (mitral valve prolapse).

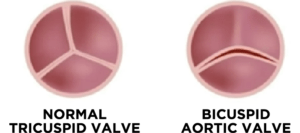
Congenital Abnormalities
People can be born with narrow, deformed, or even missing valves. For example, around 1 – 2% of people are born with a bicuspid aortic valve that has two leaflets instead of the normal three, and that typically leads to valve disease.

Infection
Bacterial endocarditis is an infection of the inner layer of the heart or heart valves that is most commonly caused by staphylococci (staph) and streptococci (strep) bacteria.
While increasingly rare in the U.S., in some countries rheumatic fever from untreated strep throat is a common cause of valve disease.

Cardiovascular Diseases and Conditions
Problems with the heart or vascular system can also result in valve problems. For example, heart attacks can cause scarring of the heart muscle and distort the valves, an enlarged heart can stretch open a valve, long-term raised blood pressure can cause heart damage, and aortic dissections or tears can extend to the valve.

Family History
Blood relatives who had/have valve disease may increase risk.

Radiation to the Chest and Certain Chemotherapy
People treated for some types of cancer require radiation therapy to the chest that can damage the valves and cause valve disease many years later. Certain types of chemotherapy can also cause valve damage.

Racism
Racism, either structural or interpersonal, negatively affects the health of people of color. The disproportionate impact of risk factors for heart valve disease on people of color is an example
of these health disparities. Black Americans experience risk factors for valve disease—such as high blood pressure and heart failure—at higher rates and at earlier ages than whites. This makes the average age of valve disease onset among Blacks younger and, as a result, more likely to go undetected and treated than in whites.

Other Health Conditions
Chronic kidney disease, lupus, and Marfan syndrome can all increase risk.
What Are the Symptoms of Valve Disease?
Valve disease reduces blood flow to the body and forces the heart to work harder, causing a number of symptoms. Many of these symptoms will only happen during exercise or activity, but as the valve disease worsens, they may also happen while resting.
Be sure to listen to your heart, pay attention to your body, and report any of the following symptoms to your healthcare provider no matter how subtle:

Lightheaded, faint, or dizzy feelings

Irregular heartbeat, heart flutter, or chest pains

Shortness of breath after light activity or while laying down

Tiredness, even if you’ve had plenty of sleep

Edema (swelling of the ankles and feet)

Not feeling like yourself (missing out on daily activities)
People with valve disease don’t always notice any symptoms, and those who do may be told or believe that these symptoms are a “normal” part of aging. While valve disease is more common with age, it is NOT an inevitable part of aging and can usually be successfully treated in patients of all ages.
How is Valve Disease Diagnosed?
Early detection and timely treatment of valve disease is critical to successful outcomes. Everyone should have their heart listened to by a healthcare provider regularly because valve disease can often be detected with a simple stethoscope check. Damaged valves often produce abnormal heartbeats and distinct sounds (murmurs) that can be heard with a stethoscope.
If a murmur is detected, your health care provider may order additional tests that can include:
- Electrocardiogram (EKG) to measure your heart’s electrical patterns
- Echocardiogram (ECG) to get sound wave images of your heart and valves
- Chest x-ray to look for fluid in your lungs or enlargement of your heart
- Cardiac magnetic resonance imaging (MRI) to create detailed images of your heart
- Exercise or stress tests with the above tools to see how the valves change or symptoms develop with exertion or when put under chemically-induced stress
- Cardiac catheterization to examine blood flow and test how well the heart and valves are functioning
Can Heart Valve Disease Be Prevented?
Many causes of heart valve disease cannot be prevented. However, a heart healthy lifestyle full of nutritious foods and physical activity, can help prevent high blood pressure and other heart conditions that can lead to valve disease. Additionally, treating known strep and staph infections can prevent complications.
How is Valve Disease Treated?
Treatment of valve disease depends on your symptoms, the severity of your disease, and whether or not it is getting worse.
Monitoring
Some types of valve disease don’t need treatment, or don’t need treatment right away. But all types should be monitored regularly to watch for progression of the disease. The frequency of recommended monitoring depends on severity of the disease. People with severe valve disease should have an echocardiogram every 6 to 12 months.
Medication
There are no medications that keep valve disease from getting worse, that undo damage already done, or that cure valve disease. However, there are some medications that can help relieve or lesson the symptoms of valve disease by reducing the heart’s workload, regulating heart rhythms, preventing blood clots, and preventing infections.
Valve Repair or Replacement
Some types of valve disease may need to be treated with valve repair or replacement. Fortunately, these procedures and surgeries are usually very successful in patients of all ages.
- Repair
If possible, the valve is repaired by modifying the structure of the valve. This can involve adding tissue to patch holes or tears, removing or reshaping tissue, separating fused valve leaflets, and more. This may require surgery or may be done through a minimally invasive procedure. - Replacement
If the valve can’t be repaired, it will need to be replaced with a new valve. The new valve can be a tissue (bioprosthetic) valve or a mechanical valve. Tissue valves are made from cow or pig tissue or taken from human cadavers. Mechanical valves are made from carbon.A valve may need to be replaced with open heart surgery—an incision is made along the chest to allow access to the heart. In some cases, the valve can be replaced through a less invasive procedure called transcatheter aortic valve replacement (TAVR or TAVI). In TAVR, a new valve is placed with a thin tube (catheter) inserted through an artery in the chest or leg.
Whether or not a valve can be repaired or replaced, if a mechanical or tissue valve is used, and if surgery or a less-invasive procedure is appropriate—depends on each patient’s health and risk factors and should be discussed between the patient and provider.
What Can I Expect After a Valve Repair or Replacement?
Most people who have valve repair or replacement can expect to return to a normal life after recovery. The amount of time for recovery varies depending on the type of repair or replacement and the health of the patient going into the procedure or surgery. Recovery times typically range from two to eight weeks—with a hospital stay of three to five days.
After a patient returns home and gets back to mild activities, they may start doing cardiac rehabilitation to help with exercise training and other support as they recover.
2022 Valve Disease Awareness Day PSA (60-second)